We parents know that steady wail. With dread, we watch for the tugging of the ears. If we ourselves have ever experienced the pain of an ear infection—part ache, part knife-sharp stab—knowing our child has one can be hard to bear.
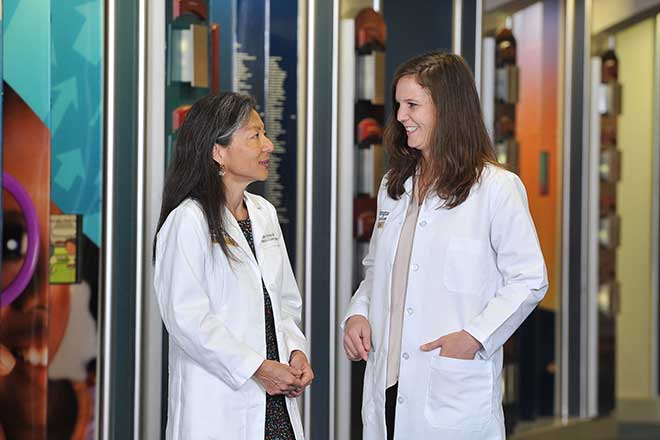
 “Ear infections are one of the most common reasons children go to the doctor,” says Dr. Keiko Hirose, Washington University School of Medicine otolaryngologist-in-chief, who divides her time between Children’s Hospital and the new St. Louis Children’s Specialty Care Center at I-64 and Mason Road. In most cases, however, the insertion of tubes (tympanostomy) is a standard outpatient procedure with excellent results.
“Ear infections are one of the most common reasons children go to the doctor,” says Dr. Keiko Hirose, Washington University School of Medicine otolaryngologist-in-chief, who divides her time between Children’s Hospital and the new St. Louis Children’s Specialty Care Center at I-64 and Mason Road. In most cases, however, the insertion of tubes (tympanostomy) is a standard outpatient procedure with excellent results.
So what are these clever devices, and how do they work? They function, Hirose explains, by allowing a controlled perforation of the eardrum and equalizing the pressure across it. Once the tube—about the size of a grain of rice and shaped like a sewing bobbin—is inserted, the pressure on the inside of the ear is the same as that on the outside. In addition, it provides an exitway for the mostly painless discharge of pus. “The bursting of an eardrum is very painful,” says Hirose’s colleague, Dr. Katherine Dunsky. “But tubes prevent that.” Another benefit is that medication can be administered successfully via drops rather than orally. “The perforation allows the medicine to pass through to the middle ear where the infection is,” says Hirose. “Otherwise, the drum acts as a barrier and drops aren’t effective.” A tympanostomy—performed under general anesthetic—takes 10 minutes and Hirose says she recommends it only after three or more infections. While adults also can be fitted with tubes, most patients, Dunsky says, tend to be 3 and under. The insertion of tubes has few side effects besides soreness and minimal, spotty bleeding.
Other common outpatient otolaryngological procedures performed at the Specialty Care Center are tonsill- and adenoidectomies. The need for these occurs when the lymphoid tissue in the throat becomes infected or enlarged, causing obstruction and difficulty breathing. The tissue, Hirose explains, relates to the immune system and, actually, functions like a lymph node. “Tonsils and adenoids are non-essential because we have other lymph nodes elsewhere in the body,” she says. Also performed under general anesthetic at the outpatient clinic, these surgeries take less than an hour. The post-operative period mostly is marked by a sore throat similar to that caused by pharyngitis.
There are four other otolaryngologists besides Hirose and Dunsky on the team, and all take turns both at the Mason Road center and at Children’s Hospital, where more serious ear, nose and throat conditions are treated. These include abnormalities of the vocal chords and voice box, tumors and cysts in the chest, and emergency procedures necessitated by choking. Dunsky says the new facility—which includes many other specialties—is unique for its breadth of services and its proximity to major highways. New to the practice, Dunsky recently has seen her first patients there.
Pictured: Dr. Keiko Hirose and Dr. Katherine Dunsky
Photo: Bill Barrett
The St. Louis Children’s Specialty Care Center is a new outpatient facility located at I-64 and Mason Road. For more information, call 314.454.6162 or visit wuphysicians.wustl.edu/pedsENT. Pictured on the cover: Dr. Katherine Dunsky and Dr. Keiko Hirose.
Cover design by Allie Bronsky | Cover photo by Bill Barrett