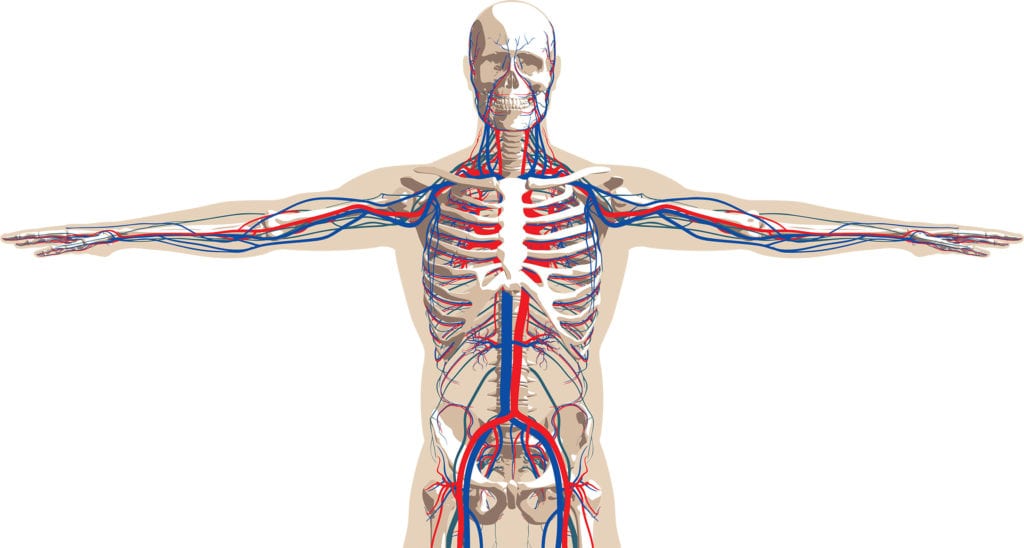
It’s never too late to improve the health of your circulatory system. Several lifestyle factors can set us up for atherosclerosis, a condition in which a waxy substance (plaque) builds up in the arteries that carry blood throughout the body. The plaque hardens and creates blockages that can lead to heart attack, stroke and even death. Heredity plays a big role, but risk can be reduced with good practices, says Dr. Norman Bein of Vein Specialties. “You can’t outrun your genes,” he says. “But exercising, avoiding tobacco and eating a balanced, low-carb diet can contribute to a long life with minimal illness.”
here’s how the circulatory system is affected by diet and lifestyle:
-
-
What happens when your diet is poor? Consuming too much processed food, salt, red meat, sugar-sweetened beverages and rapidly digested carbohydrates (like those in white bread, white rice and potatoes) can contribute to atherosclerosis and other circulatory problems. Instead, eat fruits, vegetables, whole grains and ‘good proteins’ like those in beans, nuts, fish and poultry. A low- or no-carb diet can help regulate your insulin level and your weight.
-
What happens when you drink too much alcohol? Too much alcohol can contribute to heart muscle disorders, arrhythmias, high blood pressure and stroke. If you drink, limit intake to one or two drinks a day for men, and one for women.
-
What happens when you weight is too high? Carrying extra pounds, especially around the stomach, strains the heart and increases risk for diabetes. If you’re overweight, losing just 5 to 10 percent of your body weight can have a positive impact on blood sugar, blood pressure and heart health.
-
What happens when you smoke? Chemicals in cigarette smoke can harm blood cells and damage the structure of your heart and blood vessels, increasing risk of atherosclerosis. When tobacco use is combined with other factors like unhealthy blood cholesterol levels, high blood pressure and obesity, the risk of heart disease increases.
-
What happens when you do eat right, exercise and avoid smoking? A balanced diet low in calories and saturated fat helps reduce weight and strain on the heart and blood vessels. Thirty minutes of moderate physical activity each day decreases risk of problems such as high blood pressure, stroke and diabetes. And just a year after you quit smoking, your heart disease risk drops by more than half.
deep vein thrombosis
Deep vein thrombosis (DVT) is a medical conundrum—a very serious condition that patients often don’t know they have. It causes blood clots in a vein deep inside the body or in the extremities, and about half of patients don’t show any symptoms. So they may have no idea they need medical help until a crisis occurs.
The most common location for DVT is the thigh, but it also can happen in areas like the lower leg, arm or abdomen, says Washington University vascular surgeon Dr. Mohamed Zayed. “DVT generally occurs when blood is moving too slowly through the veins and it thickens and clumps, causing a clot,” he explains. “It’s usually treated with a blood thinner. What’s most dangerous about DVT is that a clot can break free and travel to an artery in the lung, blocking blood flow to parts of it. It is known as a pulmonary embolism, and it can be very serious, even fatal.”
Patients who do experience DVT symptoms usually have discomfort, pain or swelling in the affected limb, according to SLUCare vascular surgeon Dr. Catherine Wittgen. “A physical exam isn’t enough to confirm or rule out DVT,” she says. “If it’s suspected, the patient needs an ultrasound, similar to what expectant mothers have. It can show the obstruction and changes in the vein wall, which thickens in response to the clot.”
Those who may be most at risk for DVT include bedridden patients, people who are inactive or overweight, pregnant women, and travelers who sit still for hours on long flights or car trips, Zayed says. “If you are over 40, that also increases your risk,” he notes. “The best medicine is prevention. Don’t smoke, be active every day, lose weight if needed, and when you’re on a long trip, get up and walk periodically to keep the leg muscles moving.”
Wittgen advises against trying to self-diagnose DVT by reading about it online. “You can get general information about it from reputable websites, but speak
varicose veins
In the past, doctors had to treat varicose veins with procedures like vein stripping, which could be painful and require a hospital stay. Today, they can repair the condition with outpatient therapy that needs very little recovery time, says vascular surgeon Dr. Norman Bein of Vein Specialties.
A varicose vein is a superficial blood vessel that has become twisted and enlarged because of malfunctioning valves inside it. Blood pools in the vein because the valves aren’t directing it forward efficiently through the vessel. Varicose veins can be unsightly and cause pain, swelling, fatigue and a feeling of ‘heaviness’ in the legs. If left untreated, the condition can cause additional problems like skin ulcers.
According to Bein, varicose vein treatments are considered medical procedures, so they tend to be covered by insurance. His practice treats the condition with endovenous laser ablation, an ultrasound-guided technique that takes about half an hour to perform on each leg. “We use the laser to seal affected veins and cut off their blood supply,” Bein notes. “It causes the vessel to adhere to itself and close up. The vein gets nourishment when blood is sitting in it, so it shrinks and disappears once the supply is stopped.” If vein tissue needs to be removed from the leg, Bein can do that during the same visit.
“We treat one leg at a time, usually a week apart, so patients don’t get too much local anesthesia all at once,” he explains. “We often schedule treatment at the end of the week so they can have a couple of days to rest before returning to work.” Bein says the procedure is popular among doctors, nurses, teachers, police officers and others who spend all day on their feet and may be at risk for the condition.
After treatment, patients return for a six-week follow-up visit. They may have a small amount of bruising or discomfort in the meantime, but gentle massage and ibuprofen can help, Bein notes. “Varicose vein therapy has evolved quite a bit over the years,” he says. “After treatment, patients can return quickly to a normal schedule.”
Additional sources: National Institutes of Health, Harvard Medical School