Thanks to another new technology, SLUCare physicians again are on the cutting edge of the diagnosis and treatment of cancer, specifically disorders of the blood. This time, they are using 10-color flow cytometry—capable of detecting up to 10 simultaneous fluorescent signals—to precisely depict and analyze cells from bone marrow, blood, lymph nodes and other tissue. A chief benefit of this cytometry is that diagnoses can be made in a very short time, allowing treatment to begin sooner.
Up until very recently, the cytometry instrument used two or four colors to make diagnoses, but Dr. Katherine Robbins, SLUCare patholologist and assistant professor of pathology at Saint Louis University School of Medicine, says that while that number was still very effective, the jump to more colors is akin to switching from early color television to HDTV: the picture is richer, crisper, more accurate. “It’s a highly advanced diagnostic tool,” she says of the technology, which uses lasers to map the ‘fingerprint’ of each cell. Flow cytometry is able to analyze several thousand particles a second and can acti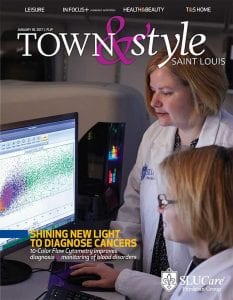 vely separate and isolate particles with specific properties. Cells are suspended in a stream of fluid and passed single file through a light beam for sensing.
vely separate and isolate particles with specific properties. Cells are suspended in a stream of fluid and passed single file through a light beam for sensing.
“In order to deliver the very best treatment, we need to understand everything about the cell. Upgrading to 10-color flow cytometry now allows us to more precisely characterize tumor cell populations,” Robbins says. An added benefit of the tool is that it can extract information from very small samples with limited cells, like those taken from fine needle aspirates, cerebral spinal fluid and small tissue biopsies. Higher information content per tube maximizes small specimens, she says, and minimizes the chance of incomplete analyses; low-frequency abnormalities can be more easily detected.
This upgrade has been in the works for several months and became available in November 2016 when live testing began. “It’s a process. We wanted to make absolutely sure the results were accurate,” Robbins explains.
She says a huge benefit of the 10-color flow cytometry is that it facilitates swift diagnoses, sometimes within a matter of hours. “In a conventional biopsy, it takes time for tissue to be processed, but now we can take live cells and run the analysis much faster,” she notes. “This has great implications since it means treatment can start sooner.” She adds that the needlepoint accuracy of the diagnosis means that oncologists can be even more precise in their decision-making regarding treatment, and that the collaboration between SLUCare doctors and departments also helps to ensure the best possible outcomes for patients. “Ours is a fully integrated service where all data is shared to provide accurate diagnoses and the best care,” Robbins says. “That’s what I believe makes SLUCare unique.”
Pictured: The 10-color flow cytometry facilitates swift diagnose, sometimes within hours.
Photo courtesy of SLUCare Physician Group
SLUCare Physician Group Hematopathology Flow Cytometry Laboratory now offers the high-tech 10-color flow cytometry. Capable of detecting more than 10 simultaneous fluorescent signals, the cytometer improves the diagnosis and monitoring of blood disorders. Pictured on the cover, standing: SLUCare pathologist Katherine Robbins, M.D., director of the Flow Cytometry Laboratory. Seated: Nichol Reeves, flow cytometry technologist. Fore more information, visit slucare.edu/10flow.
Cover design by Julie Streiler | Cover photo courtesy of SLUCare Physician Group