In sleep, our hearts and brains rest. The beats become fewer, the waves become slower. Without sleep, our vital organs have no chance to recuperate. This is why, says Dr. Raman Malhotra, co-director of the SLUCare Sleep Disorders Center, untreated obstructive sleep apnea (OSA) can be very detrimental to health, and sometimes even fatal. “If it goes undiagnosed, it either can cause the kind of sleepiness that makes certain everyday activities like driving dangerous, or it can lead to heart attacks and other life-threatening conditions,” he says. “A lack of good sleep puts tremendous stress on organs.”
Obstructive sleep apnea—which affects 12 percent of the population—is caused by obstruction of the upper airway and is characterized by pauses in breathing during sleep due to relaxed throat muscles. Malhotra says physicians are seeing more cases as obesity rates rise and people live longer. Both conditions increase the risk of OSA. Add alcohol consumption to that, and the prognosis can worsen.

But how do we know for certain we have OSA, when possible symptoms like snoring or snorting in sleep aren’t always reliable indicators? Sometimes, snoring is just snoring,” Malhotra says. “But sometimes, it may indeed be a sign that air is trying to get through.”
SLUCare Sleep Disorders Center patient James Snell says his wife alerted him to the problem. “I was keeping her awake. She told me I snored badly and although I sometimes woke myself up doing so, I didn’t realize how bad it was,” he says.
Until recently, testing for OSA took place only in SLUCare’s Sleep Disorders Center, where patients spend the night hooked to 20 or more sensors. In the last few years, however, SLUCare has been issuing home test kits to patients. The doctor points out that not only is this a less-expensive, more immediate option, but it also allows people to sleep in their own beds and is particularly advantageous for home-bound, elderly or chronically ill people. While there are many benefits to a home test, it is a less-thorough diagnostic tool, and for some patients, additional testing may be required.
So what treatments are available for sufferers, and how successful are they? Malhotra says the most common course of action is CPAP (continuous positive airway pressure) delivered via a machine to the upper airways. Similar to an oxygen mask, the device fits over the nose and mouth and keeps the passages open by delivering a constant pressurized stream of warm, humidified air. The masks come in all shapes, sizes and materials. “It’s like finding the right shoe that fits,” Malhotra notes. “But once you do, CPAP can be very effective.”
Snell, who was diagnosed with OSA after a night in the sleep center, is a CPAP success story: “When they wired me up to all those sensors, they could see I actually stopped breathing. My sleep was broken, and they were worried I wasn’t getting enough rest,” he explains. “I’ve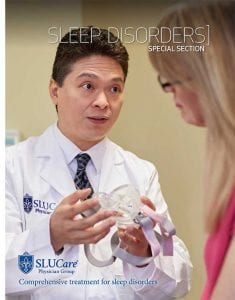 been using that machine
been using that machine
for five years, and it’s a wonderful thing.” Snell says a life spent scuba diving may have made him a particularly good candidate for CPAP, but adds that either way, it doesn’t take long to get used to it. “You just have to relax a little and breathe,” he says. However, Malhotra says it’s not for everyone, which is why SLUCare offers an ‘alternatives to CPAP clinic,’ where doctors of different specialties collaborate to find other solutions. One possibility, Malhotra says, is a mandibular advancing device (MAD), a custom-made dental appliance that fits in the mouth and keeps the lower jaw and tongue forward. This prevents the airway from collapsing and can be up to 75 percent effective for mild to moderate sleep apnea, he explains. The CPAP alternatives clinic refers patients to community dentists for fitting.
But in the event that neither CPAP nor MAD is possible, what else is there? “There still are options,” Malhotra says. “We also can look at possible surgical solutions.” These, he says, would be considered in more severe cases of OSA, where there’s an overcrowding of the airway due to larger-than-normal tonsils or adenoids. More often, space is compromised by an enlarged uvula, in which case a uvulopalatopharyngoplasty (a surgery to remove or reshape throat tissue) is recommended.
In advance of this careful procedure, SLUCare otolaryngologists conduct a nasal pharyngoscopy, involving a camera on the end of a tiny tube. “The throat area is numbed and patients don’t feel it a bit,” Malhotra says. The exam, he says, also determines whether the tongue might be interrupting air passage and needs to be reshaped as well. “The beauty of the clinic is that it’s a one-stop shop,” Malhotra concludes, citing the fact that clinicians also collaborate with weight loss experts if weight is seen to be an issue, and can address sleeping positions, where relevant. Malhotra stresses that a good night’s sleep is one of the secrets to a healthy life. At the SLUCare Sleep Disorders Center, he and his colleagues work tirelessly to get their patients the rest they need.
Pictured: Neurologist and sleep medicine specialist Dr. Raman Malhotra
Photos courtesy of SLUCare Physician Group