Usually when people hear the term HPV (human papillomavirus), they think of something that causes cervical cancer in women. But HPV is an important concern for men as well, says SLUCare otolaryngologist and surgeon Dr. Greg Ward, who practices at SSM Health Saint Louis University Hospital.
The same group of HPV viruses responsible for cervical cancer can lead to oropharyngeal cancer that mainly affects men, according to Ward. “It’s a cancer of the tonsils or base of the tongue,” he says. “About 80 percent of oropharyngeal cancer patients are male, and the first sign is often a painless neck mass. Most patients tell us they’ve noticed it for a couple of weeks, but it likely has been there much longer.” Ward says oropharyngeal cancer can appear as a large tumor or smaller ones that metastasize (spread) in the neck and may be harder for patients to detect. “They first notice it as a growth behind the angle of the jaw, not a tongue- or tonsil-based problem,” he says. “They also may have trouble swallowing, unexpected weight loss and referred pain in the ear or throat.”
 Most research shows that sexual contact is the main avenue of transmission for HPV strains that cause oropharyngeal cancer, according to Ward. “Frequent sexual activity beginning at an early age can put you at higher risk,” he says. “Nearly everyone is exposed to HPV at some point. Six or seven percent of the population develops a persistent HPV infection, and a small subset of those people develop cancer. Still, it’s important to talk about, and prevention is the best approach for both sexes.” In fact, statistics suggest oropharyngeal cancer soon will be more common than cervical cancer, Ward adds. According to CDC data, oropharyngeal cancer has risen steadily in the U.S. over the past decade and a half, with about 15,000 men now diagnosed each year.
Most research shows that sexual contact is the main avenue of transmission for HPV strains that cause oropharyngeal cancer, according to Ward. “Frequent sexual activity beginning at an early age can put you at higher risk,” he says. “Nearly everyone is exposed to HPV at some point. Six or seven percent of the population develops a persistent HPV infection, and a small subset of those people develop cancer. Still, it’s important to talk about, and prevention is the best approach for both sexes.” In fact, statistics suggest oropharyngeal cancer soon will be more common than cervical cancer, Ward adds. According to CDC data, oropharyngeal cancer has risen steadily in the U.S. over the past decade and a half, with about 15,000 men now diagnosed each year.
Ward says because people often mistakenly associate HPV solely with women, there can be barriers in men’s awareness, prevention and early detection. “The HPV vaccine can be given to boys to help prevent oropharyngeal cancer,” he notes. “Women get Pap smears to look for HPV-related cell changes during gynecological exams, but men don’t have the same regular framework for screening. If men believe HPV is only a female issue, they may miss an opportunity for early diagnosis.”
Ward says the key to reducing cancer rates is for parents to educate themselves and their families about prevention. “If you are old enough to be a parent, you likely are already outside the age range to get the vaccine yourself,” he notes. “So it’s even more important to talk to your doctor about having your children vaccinated.” Ward and his SLUCare practice partner, Dr. Ronald Walker, perform head and neck cancer evaluations and take referrals from doctors across the area. He says they are committed to getting the word out about this growing health concern.
“We know that a mass in the neck is cancerous in adults about 80 percent of the time,” he says. “It’s important for at-risk men to be evaluated regularly for oropharyngeal cancer. You don’t want to delay a diagnosis that could increase your chances for a positive outcome.”
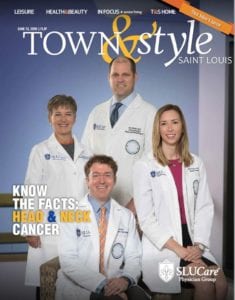
SLUCare Physician Group provides comprehensive, personalized care for cancer patients. Pictured on the cover, clockwise from left: Family nurse practitioner Carole McKinstry, Dr. Ronald Walker, speech-language pathologist Michelle Payne, Dr. Greg Ward. For more information, call 314.977.5110 or visit slucare.edu/head-neck-surgery.
Cover design by Julie Streiler
Cover photo courtesy of SLUCare Physician Group
Pictured above: Dr. Greg Ward works with a patient.








