 In the past, cancer patients with tumor damage to bone structures like the pelvis might need invasive surgery to correct the defect, and recovery was likely to be long and challenging. It might even delay the patient’s chemotherapy or radiation treatment for a period of time, explains SLUCare orthopedic oncologist Dr. David Greenberg. Newer surgical methods are much less invasive and disruptive, however, and patients reap a number of benefits including a shorter, easier recovery period.
In the past, cancer patients with tumor damage to bone structures like the pelvis might need invasive surgery to correct the defect, and recovery was likely to be long and challenging. It might even delay the patient’s chemotherapy or radiation treatment for a period of time, explains SLUCare orthopedic oncologist Dr. David Greenberg. Newer surgical methods are much less invasive and disruptive, however, and patients reap a number of benefits including a shorter, easier recovery period.
One of the latest techniques Greenberg uses is a combination of radiofrequency ablation and an implant system called IlluminOss, which can help stabilize the bone and prevent fractures. A real-time navigation system allows the surgeon to achieve precise results during surgery, and only small incisions are typically required. Greenberg says the technique is particularly helpful in older patients, who may develop problems like physical weakness and blood clots if they can’t move around normally.
High Ridge resident Loretta Peters, 86, had the procedure done at SSM Health Saint Louis University Hospital, and she feels grateful for the results she has seen. “I used to have a good deal of pain and loss of motion in my leg, but the discomfort is just about gone,” she says. “Without the procedure, I probably would have ended up in a wheelchair, but now, I can get around without a walker and am nearly back to my normal routine. Before I had surgery, my daughter had to do most of the work around the house, but I’ve returned to cooking, making beds, doing laundry and even some shopping. I had just three small incisions, stayed in the hospital less than 24 hours, and went home. It’s remarkable how fast I’ve gotten better.”
Greenberg says the radiofrequency ablation and IlluminOss procedure is one of SLUCare’s newest and most successful strategies to improve quality of life for cancer patients. “People, tumors and health situations are all unique, but this has become a preferred method of treatment for me in cases where it’s appropriate, and SLUCare is one of just a few local providers to offer the technology,” he says. “It’s always rewarding when we can help a patient avoid more invasive surgery and get back to normal activities faster.” He says older procedures could take 8 to 12 hours to perform, potentially requiring an ICU stay and up to two weeks in the hospital.
Greenberg says the cancers that most commonly metastasize to bone include those of the breast, lung, thyroid, kidney and prostate. SLUCare physicians work carefully with each patient to determine needs, goals and an appropriate plan, and he says it’s extremely satisfying to see the positive results they experience. “Loretta went from being nonmobile to asking us if she could start taking yoga,” he notes. “That’s a pretty significant change.”
Peters says she can’t express appreciation for her care enthusiastically enough. “Dr. Greenberg and the staff are wonderful to work with,” she says. “It can be hard to know what to do when you’re faced with a health problem, but they gave me the courage to say yes to the procedure, and I’m so glad I did. I can’t believe the difference it has made.”
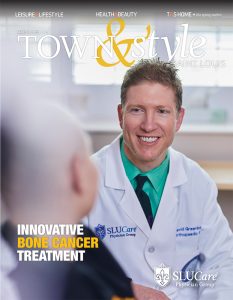
SLUCare physicians offer precise, personalized care for patients with cancers that affect bone and soft tissue health. Pictured on the cover: SLUCare orthopedic oncologist Dr. David Greenberg. For more information, visit slucare.com.
Cover design by Julie Streiler
Cover photo courtesy of SLUCare Physician Group
Pictured at top: SLUCare orthopedic oncologist Dr. David Greenberg works with a patient.
Photo provided by SLUCare Physician Group