Despite recent  discussion about who should get mammograms and how often women need them, breast imaging saves lives. Beyond that, patients need to decide where to get their mammograms and what type is necessary for them. That’s where the expert opinions come in.
discussion about who should get mammograms and how often women need them, breast imaging saves lives. Beyond that, patients need to decide where to get their mammograms and what type is necessary for them. That’s where the expert opinions come in.
imaging update
“We can pick up cancer on a mammogram as early as two years before it can be felt,” says Dr. Cara E. Hahs, breast surgeon at Mercy Breast Surgery Clinic. “We know that mammograms save lives—that is well-documented.” Do we really need more convincing than that?
scary stats
One in eight American women will develop breast cancer, and nearly one-third of female cancers is in the breasts. Sobering statistics. The good news is that the mortality rate for breast cancer in the U.S. has declined by about a third since 1975. Yet conflicting guidelines have women questioning their options.
“Confusing guidelines have been reported,” says Dr. Catherine M. Appleton, chief of breast imaging in the division of diagnostic radiology at Washington University School of Medicine and Siteman Cancer Center.
“We know that if we can catch breast cancer at an early stage, primarily defined as when it is confined to the breast tissue, it is much more treatable and people have a better prognosis,” says Mercy’s Hahs.
mammography vs. tomosynthesis
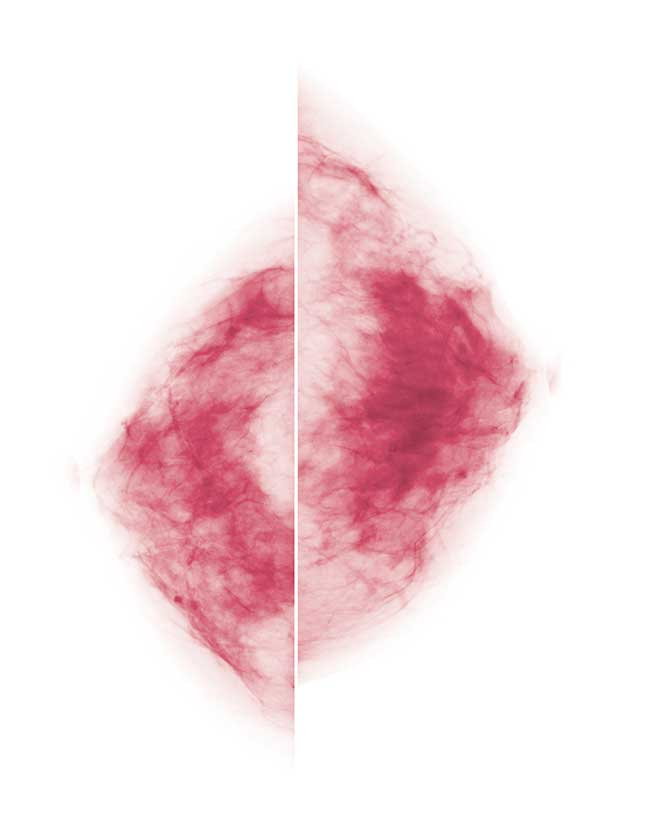
“The other hot topic is the three-dimensional mammogram, which is called tomosynthesis,” Hahs says. Both 2-D and 3-D images can find cancer when it is in the form of calcifications, which are almost like grains of sand, Appleton says. “That is a victory for mammography because those cancers are not invasive yet.”
But tomosynthesis, 3-D imaging, magnifies the clarity of the examination, creating images of all breast tissues as seen from one view—somewhat like peering through all the pages of a closed book at one time, Appleton explains. “With tomosynthesis, we create a volume of data. We literally can page through the breast in 1-millimeter slices (a millimeter is thinner than a dime).”
There’s no question that 3-D imaging exposes abnormalities that couldn’t be seen before, Appleton says. And it minimizes the need for call-back exams. “Women with dense breasts are good candidates for tomosynthesis mammograms,” Hahs adds. “Insurance companies vary on what they will pay for. Some are completely on board and some are not.”
other factors
“I would like women to ask about the technology that is being offered to them and also about who is reading the mammogram,” Appleton says. “Having a radiologist who specializes in breast imaging arguably is going to improve interpretation.” Training for radiology requires five years beyond medical school, she says, and “then becoming sub-specialized in breast imaging is an additional year of training. We are behind the scenes, but what we do is important for patients.”
There are other abnormalities that can be better detected with 3-D imaging, namely ‘architectural distortion,’ a medical way of saying the tissue pattern in the breast looks different than it should, explains Dr. Debbie Bennett, SLUCare breast radiologist and director of breast imaging for SSM Health at Saint Louis University Hospital.
And last, but not least, it’s important to remember that breast cancer is very treatable, Hahs says. “More than 95 percent of women who are diagnosed in an early stage, through something found on a mammogram, are alive and disease-free five years later.”
 evolving technology
evolving technology
We in St. Louis are fortunate to live in a medical mecca. With top-ranked medical centers, we have access to the latest in diagnosis and treatment. This not only saves lives, but also reduces anxiety and improves quality of life.
high tech
The most comprehensive form of breast imagery is the 3-D variety, which uses ultrasound to detect abnormalities that are still tiny specks or hidden in dense tissue. “Tomosynthesis allows us to see multiple slices through the tissue,” says Dr. Deborah Wadsworth, a radiologist at The Breast Center at Mercy Hospital. “A 2-D image (the typical 2-D mammogram) can miss a lot of details. Three-dimensional imaging is like flying through this very dense forest and seeing every tree. We can take the computer mouse and scroll back and forth and around the image.”
In August, SSM Health and Saint Louis University Hospital became the first breast center in the U.S. to offer technology that provides 3-D-guided breast biopsies for patients in a prone position. It’s a procedure approved by the U.S. Food and Drug Administration in April called Affirm Prone Biopsy System.
Previous equipment required that patients sit upright while undergoing a needle biopsy guided by 3-D mammography, explains Dr. Debbie Bennett, director of breast imaging for SSM Health at Saint Louis University Hospital. “It is problematic to do a biopsy that way because even if you close your eyes or turn your head, it is very difficult not to peek down and see what is happening.” She reports that patients sometimes passed out during the procedure.
improvements all around
The Affirm imaging and biopsy process offers women a much less invasive and intimidating option. The equipment is based under a padded table with an opening in the middle. “The woman positions her breasts and a needle biopsy is done through the skin under local anesthesia,” Bennett says. “We take a few little samples. You essentially get a Band-Aid, a little bit of surgical glue and no stitches.” Affirm is not used for everything because ultrasound-guided biopsies are better under certain conditions.
The Mercy Breast Center received a new 3-D ultrasound machine in September, which is much improved over earlier generations of ultrasound. “It performs an examination of the entire breast and is automated,” Wadsworth explains. “A few years ago the computer algorithms weren’t ready. It is starting to hit its stride.”
Ultrasound is the mode of choice for women with dense breasts, she says. “They have glandular tissue that obscures smaller tumors on the (X-ray) mammogram. We are better able to see some tumors on ultrasound and other tumors with mammography.”
The ultrasound examination is rated by some women as less uncomfortable, as well, Wadsworth reports. “For the 3-D ultrasound, patients lie on their back, and a curved paddle is placed on the breast in three positions, then a wand goes over the breast,” she explains. “It’s more like an intensive massage.”
success rates
Both 3-D ultrasound imaging and X-ray mammograms detect tumors at about the same rate, Wadsworth notes. “The hope is that as we increase our detection rate, we will pick up cancers before they get larger and are palpable.” And there’s more good news for breast cancer patients, according to Bennett. “Technology over the past 10 years has gotten so much better that the percentage of cancers detected at an early stage is already very high,” she says.
reconstruction options
Breast cancer sometimes brings with it a host of new and different issues when a woman loses a breast (or both of them) to the disease. Should reconstruction be planned at the time of removal? If so, how should it be done? If not, what is the alternative plan?
first things first
The first decision is whether to do a reconstruction at all, says Dr. Terry Myckatyn, a surgeon at West County Plastic Surgeons of Washington University. “Every woman needs to weigh her biases, goals and priorities with her medical situation—the type of cancer she has, her body and her shape. It is a very complex decision.”
Women often dela y reconstruction until they have healed from the initial surgery, but sometimes it is advantageous to perform some or all of a reconstruction during the first trip to the operating room, Myckatyn says.
y reconstruction until they have healed from the initial surgery, but sometimes it is advantageous to perform some or all of a reconstruction during the first trip to the operating room, Myckatyn says.
About 40 percent of women across the U.S. choose reconstruction after a mastectomy, Myckatyn notes. “At Siteman Cancer Center, the rate is 60 to 70 percent. I think breast reconstruction is under-offered in rural settings because of difficulty with scheduling, lack of a plastic surgeon or knowledge by the provider, or lack of insurance reimbursement.” He adds, though, that reconstruction following cancer surgery “is covered by insurance by law.”
implants vs. native tissue
“We can use implants or the woman’s own tissue,” Myckatyn says. “More women get implants because the operation is less invasive, but there are several good reasons to use your own tissue.” For one thing, artificial implants are more prone to infections, can prompt development of scar tissue and may leak. “They are good devices but eventually, they will fail,” Myckatyn says. If the patien’ts own tissue is used, it comes from another part of the body, like the belly, back, inner thigh or buttocks.
The procedure now used to harvest tissue, the DIEP flap, requires less recovery time than the previous procedure because it does not remove muscle, Myckatyn says. “It is very similar to the tissue removal for a tummy tuck. There still can be some abdominal weakness, but there tends to be less.”
different cancers, different options
Reconstruction options can vary depending on the form of breast cancer: mastectomy (removal of all breast tissue) or lumpectomy (removal of the tumor and some portion of breast tissue). “We prefer to do surgery at the same time as a lumpectomy if we can,” Myckatyn says. “Almost everybody who has a lumpectomy gets radiation. We can still do surgery after radiation, but it tends to be a bit more complicated and there is increased risk of a wound problem or infection.”
Mastectomy reconstruction options depend on the required surgical procedure and the woman’s physical shape and health, he says. “More often these days, we are doing a nipple-sparing mastectomy. It makes the reconstruction much prettier and sometimes we can put in an implant right away.”
The good news is in nearly all cases, women who have breast reconstruction can expect to look ‘normal’ afterward.