Brittany Franklin wasn’t expecting a diagnosis of ulcerative colitis (UC) at the age of 22. She was just embarking on her adult life, looking forward to a bright future. But when intestinal problems landed her at Barnes-Jewish Hospital, she had to confront a new health reality.
UC is an inflammatory bowel disease (IBD) that creates sores in the wall of the large intestine. Doctors aren’t sure what causes UC, a type of autoimmune condition, says Washington University gastroenterologist Dr. Matthew Ciorba. The main symptoms include serious abdominal pain, cramping and diarrhea that is sometimes bloody. The condition’s psychological and social effects can be just as tough to handle as its physical ones, he says. Patients worry about flare-ups, and often feel they have to stay at home or keep close to a restroom at all times.
“I started seeing Dr. Ciorba after being admitted to the hospital,” Franklin says. “At the time, my disease was pretty severe, so he recommended a combination of steroids, an immunosuppressant, and eventually a biologic IV infusion.” She initially was concerned about possible side effects of the infusion—infection and a small increased risk of certain types of cancer, among other things. But Ciorba discussed the risks and rewards openly, along with a proactive monitoring plan, and Franklin decided to begin therapy. “He explained that my options were that or colon surgery,” she notes. “After a year of infusion therapy, I was able to come off the steroids and immunosuppressant.”
 Ciorba says as many as 3 million Americans have IBD, a category that also includes Crohn’s disease. Crohn’s can cause inflammation, ulcers and bleeding anywhere along the gastrointestinal tract, whereas UC is limited to the large intestine. Both diseases show up most often in the late teens and early 20s, Ciorba notes, but they can appear later in life as well. Because they are linked to increased colon cancer risk, it’s important to see a doctor if symptoms appear. When IBD patients come in, the Washington University team runs thorough diagnostic tests and creates a personal treatment, diet and lifestyle plan to keep symptoms under control, Ciorba says. IBD patients also have access to a gastrointestinal-health psychologist and nutritional counseling.
Ciorba says as many as 3 million Americans have IBD, a category that also includes Crohn’s disease. Crohn’s can cause inflammation, ulcers and bleeding anywhere along the gastrointestinal tract, whereas UC is limited to the large intestine. Both diseases show up most often in the late teens and early 20s, Ciorba notes, but they can appear later in life as well. Because they are linked to increased colon cancer risk, it’s important to see a doctor if symptoms appear. When IBD patients come in, the Washington University team runs thorough diagnostic tests and creates a personal treatment, diet and lifestyle plan to keep symptoms under control, Ciorba says. IBD patients also have access to a gastrointestinal-health psychologist and nutritional counseling.
Ciorba adds that IBD unfortunately can come with a fair amount of stigma, which makes it difficult for patients to ask for help, but they shouldn’t be afraid to speak up. “These are complex diseases, but there is increased awareness over the last decade,” he says. “New medications and treatments are being developed to offer better quality of life. And our Washington University researchers are among the leading investigators in IBD-related genetics. Connecting clinicians with scientists allows us to expand our patients’ options.”
Franklin says her UC now has been in remission for six years. She still takes a daily medication and has infusion therapy every other month, but is grateful to have avoided surgery. She’s feeling good and expecting her second child, and says she truly appreciates the caring help of Ciorba and his staff. “I can’t say enough about them,” she notes. “They guided me to do what was best for me and my family.”
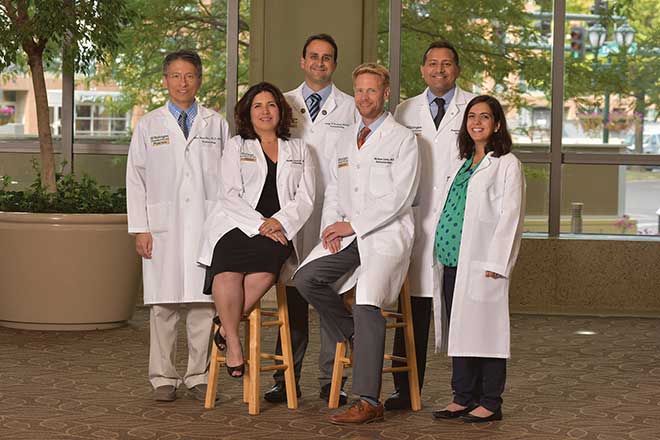
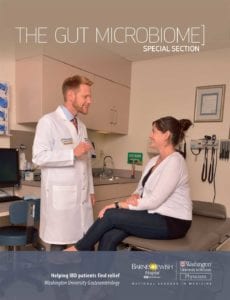
Washington University Physicians offers comprehensive and compassionate care for patients with IBD. They can be seen at three St. Louis-area locations and work with multidisciplinary experts who provide whole-patient care. Pictured on the cover: Dr. Matthew Ciorba with a patient. For more information, call 314.747.IBD6 (4236) or visit gastro.wustl.edu/IBD.
Pictured at top: Washington University IBD specialists Chien-Huan Chen, M.D., Ph.D.; Alexandra Gutierrez, M.D., MPH; George Christophi, M.D., Ph.D.; Matthew Ciorba, M.D.; Parakkal Deepak, MBBS, MS; Cynthia Cherfane, M.D.
Cover provided by Washington University Physicians
Photos: Mark Gilliland